(Image source from iStock & Illustrations by Jason Hoffman)
By Krista DeMaio
You’re working with your doctor and taking your meds.
What else can you do to ease psoriatic arthritis aches and pains?
A lot. It’s time you deserve some…Sweet Relief
Psoriatic arthritis (PsA) can feel a lot like having two diseases at once. (Lucky you!)
 You may get red, scaly, painful plaques on your skin (as seen with psoriasis) and arthritic joint pain. But here’s the thing: PsA is different from both psoriasis and other types of arthritis. It’s a unique condition with inflammation driving both skin and joint pain, says Rebecca Haberman, M.D., clinical instructor of rheumatology at NYU Langone Health in New York City. PsA is also an autoimmune condition, which means your body turns against its healthy tissue. The result is inflammation that manifests in your joints and their surrounding ligaments and muscles, as well as your skin. In most cases, the skin patches (a.k.a. plaques) appear first. But some folks get joint and muscle pain long before they see scales.
You may get red, scaly, painful plaques on your skin (as seen with psoriasis) and arthritic joint pain. But here’s the thing: PsA is different from both psoriasis and other types of arthritis. It’s a unique condition with inflammation driving both skin and joint pain, says Rebecca Haberman, M.D., clinical instructor of rheumatology at NYU Langone Health in New York City. PsA is also an autoimmune condition, which means your body turns against its healthy tissue. The result is inflammation that manifests in your joints and their surrounding ligaments and muscles, as well as your skin. In most cases, the skin patches (a.k.a. plaques) appear first. But some folks get joint and muscle pain long before they see scales.
The cause of PsA is unknown, but genes seem to play a large role, as well as having a personal and family history of psoriasis. It’s estimated that 30% of those with the inflammatory skin condition also have PsA. Many people will have psoriasis for about a decade before their PsA flares up.
It’s estimated that 30% of those with psoriasis also have PsA.
 Your doctor likely has you on a drug regimen that matches the severity of your disease. Some people are more affected on the skin; others feel pain in multiple joints. “Psoriatic arthritis typically affects the large joints, especially those of the lower extremities (such as knees), distal joints of the fingers and toes (that look like swollen sausages), and it also can affect the back and sacroiliac joints of the pelvis,” says Amir Barkhodari, M.D., a rheumatology fellow at Stony Brook Medicine in Stony Brook, NY.
Your doctor likely has you on a drug regimen that matches the severity of your disease. Some people are more affected on the skin; others feel pain in multiple joints. “Psoriatic arthritis typically affects the large joints, especially those of the lower extremities (such as knees), distal joints of the fingers and toes (that look like swollen sausages), and it also can affect the back and sacroiliac joints of the pelvis,” says Amir Barkhodari, M.D., a rheumatology fellow at Stony Brook Medicine in Stony Brook, NY.
“The recommended therapy can be different for everyone, but the goal is always to bring down that inflammation,” says Dr. Haberman. So, your doc has that part covered, but flares can still happen even when you’re on meds, and you can still wind up with swollen joints that cause pretty debilitating pain. Plus, a flare can leave you feeling wiped out because your body spends so much energy fighting itself. “When you’re really inflamed, you may feel like you need a nap in the middle of the day,” says Dr. Haberman. Fortunately, there are things you can do to manage the life-disrupting side effects of PsA. From stretches that increase your range of motion to hacks for a more restful night sleep, here’s how to show your PsA some TLC at home.
Moving your body may be the last thing you feel like doing, but stiffness, fatigue and muscle weakness stem from not moving enough.
– Amir Barkhodari, M.D.
The Best Morning Stretches for Psoriatic Arthritis
Getting up and at ’em can be especially tough when you’re experiencing a flare. Many think PsA and other arthritic conditions only affect your joints, but the inflammation also stiffens the ligaments and surrounding muscles, says Eliana Cardozo, D.O., assistant professor of rehabilitation medicine at The Icahn School of Medicine at Mount Sinai Hospital in New York City. Taking a few minutes every morning to stretch affected areas can loosen those muscles and ligaments, which means less stress on your joints, and an increase in range of motion. These five soothing stretches are expert-approved for PsA pain. Give them a try.
1. Cat/Cow
 If you’ve ever taken yoga, you know this spine stretch. Begin by finding a soft rug or using a yoga mat and getting down on all fours.
If you’ve ever taken yoga, you know this spine stretch. Begin by finding a soft rug or using a yoga mat and getting down on all fours.
- As you breathe in, put an anterior tilt in your lower back (read: arch your back).
- Lift your head and raise your eyes toward the ceiling.
- Then reverse the curve of your back with a posterior tilt, drawing your belly button into the spine, and breathing out.
- As you round your back, drop your head towards the floor. “It’s a really nice, gentle stretch for the back,” says Cardozo.
2. Scapular Squeeze
 This move is good for someone with upper back pain from PsA. It both stretches and strengthens ligaments and muscles.
This move is good for someone with upper back pain from PsA. It both stretches and strengthens ligaments and muscles.
- Start by sitting or standing with your arms relaxed at your sides.
- Then pull your shoulders back, squeezing them together and pretending you’re pinching a pencil in between your shoulder blades. (Top tip: Don’t hunch or raise your shoulders as you do this.)
- Hold for five seconds and then relax. “It helps strengthen your upper back and postural muscles, but also stretches out your chest muscles,” says Cardozo.
3. Neck stretch
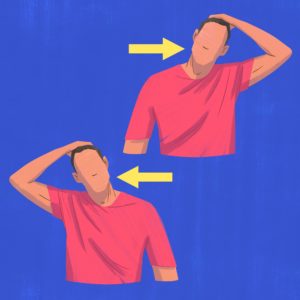 Here’s one to loosen a stiff neck and upper back.
Here’s one to loosen a stiff neck and upper back.
- Start by standing tall, feet hip-width apart.
- Raise your left arm straight up in the air, then bend your left elbow and reach your left hand over the top of your head until it touches the right side of your forehead; gently tug your head toward the left until you feel a stretch in neck muscles and shoulder.
- Hold for a few seconds. Then gently release and repeat on the other side.
4. Core Engagement
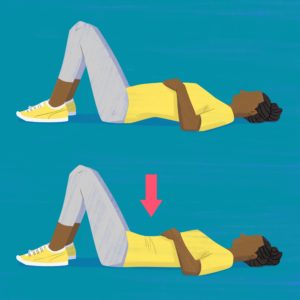 Core muscles support the spine, so strengthening them can help keep your spine in alignment, which means less stress on your spine joints. To strengthen your core, try this move:
Core muscles support the spine, so strengthening them can help keep your spine in alignment, which means less stress on your spine joints. To strengthen your core, try this move:
- To begin, lie on your back with knees bent, feet flat on the floor. Let your arms relax by your sides.
- Place your hands on your ribcage and inhale deeply, feeling your chest rise toward the ceiling.
- Then as you exhale, draw your belly button into your spine and press the small of your back into the floor, feeling your abdominal muscles engage.
- Hold for five seconds. Release and repeat.
5. Finger Stretch
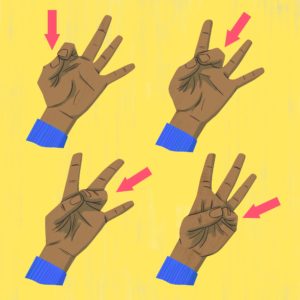 PsA often affects hands. One-third of people with PsA have dactylitis, or swelling of the fingers. These moves for your digits help with stiffness and mobility.
PsA often affects hands. One-third of people with PsA have dactylitis, or swelling of the fingers. These moves for your digits help with stiffness and mobility.
- Hold your hand palm up and fingers extended. Take your index finger and press it against your thumb (leaving all the other fingers extended).
- Hold for a few seconds. Release and do the same with your middle finger, working your way down until you’re connecting your pinky and thumb.
- Repeat a few times and switch hands.
Secrets to Sleeping with Less Pain
If aching joints and inflamed, itchy skin are keeping you up at night, you’re not alone. Research has shown that 84% of people with PsA have poor sleep quality. Here, six hacks for better shut eye.
- Wear loose-fitting, comfy pajamas. Anything too tight and constricting can irritate skin plaques and rashes. Natural fibers such as cotton and silk are especially lightweight and gentle as compared to many synthetic fibers, says Joshua Zeichner, M.D., director of cosmetic and clinical research in dermatology at Mount Sinai Hospital in New York City.
- Position pillows for pain. If you have lower back pain and you sleep on your side, slip a pillow between your legs, says Cardozo. If you sleep on your back, slip a pillow or a roll under your knees. The extra support takes some of the pressure off your spine.
- Enroll in a sleep study. A study published in the Journal of Clinical Sleep Medicine found a link between psoriasis and sleep apnea, a condition marked by brief moments of not breathing through the night. PsA is also associated with restless leg syndrome, which causes an uncontrollable and unconscious urge to move your legs while you sleep. If you’re more fatigued than usual during the day, talk to your physician about a sleep study. Addressing any underlying conditions can help you catch better zzz’s.
- Take a warm (not hot) shower. Time spent under a warm spray can help loosen stiff muscles before bed and help you feel more relaxed. Just don’t turn the dial to hot or you’ll risk irritating your skin and increasing inflammation. “Set the temperature of your shower to what you’d imagine a heated pool would feel like in the summer,” says Dr. Zeichner. And limit shower time to 10 minutes.
- Soothe cranky skin. If you have a flareup, apply a rich ointment or balm to make irritated, inflamed skin feel more comfortable before you hit the sheets. Look for one that’s fragrance-free (perfumes can irritate skin even more) and that contain emollients such as petrolatum ceramides, shea butter, or plant oils (which make a product easy to apply). Dr. Zeichner suggests Vaseline Intensive Care Advanced Repair Lotion, $7.
- Make meditating part of your routine. Those with PsA are more prone to stress and depression, which can interfere with sleep. This, in turn, becomes a vicious cycle because these mental health issues can make PsA worse. Interrupt that cycle with a calming meditation practice (keep scrolling to watch our how-to video, below) every night to help you wind down before bed.
There is a huge body of research demonstrating that meditation and other mindfulness practices reduce inflammation.
– Dr. Stacie Stephenson
Easy At-Home Pain Relievers
Non-Steroidal Anti-Inflammatory Drugs (NSAIDs)
 Your PsA prescription drugs should reduce inflammation, but since flares can occur even when you’re on meds, sometimes you’ll need “rescue medications,” says Dr. Haberman. The main ingredient in these drugs is typically ibuprofen. Common examples of NSAIDs are Advil, Motrin, and Naproxen. But, like all meds, they’re not without side effects. Run things by your doctor before popping one of these pills to make sure there are no contraindications with your other medications, or that you don’t have any other risk factors such as a cardiovascular issue.
Your PsA prescription drugs should reduce inflammation, but since flares can occur even when you’re on meds, sometimes you’ll need “rescue medications,” says Dr. Haberman. The main ingredient in these drugs is typically ibuprofen. Common examples of NSAIDs are Advil, Motrin, and Naproxen. But, like all meds, they’re not without side effects. Run things by your doctor before popping one of these pills to make sure there are no contraindications with your other medications, or that you don’t have any other risk factors such as a cardiovascular issue.
Hot/Cold Therapy
 “If a joint is actively inflamed, ice and heat can make it feel better even just temporarily,” says Dr. Haberman. Ice helps with swelling and soreness, while heat, from, say, a heating pad or hot compress, helps loosen tight muscles. These offer quick relief but know these aren’t going to do anything f or the underlying inflammation. Don’t apply heat or ice directly to your skin; use a bag or piece as a cloth to temper the effects of the extreme temps on your skin, says Haberman. You can use ice packs, heating pads, store-bought compresses—whatever feels comfortable to you—for 15 minutes at a time.
“If a joint is actively inflamed, ice and heat can make it feel better even just temporarily,” says Dr. Haberman. Ice helps with swelling and soreness, while heat, from, say, a heating pad or hot compress, helps loosen tight muscles. These offer quick relief but know these aren’t going to do anything f or the underlying inflammation. Don’t apply heat or ice directly to your skin; use a bag or piece as a cloth to temper the effects of the extreme temps on your skin, says Haberman. You can use ice packs, heating pads, store-bought compresses—whatever feels comfortable to you—for 15 minutes at a time.
Mindfulness
 Practice mind over matter to decrease pain. “There is a huge body of research demonstrating that meditation and other mindfulness practices reduce inflammation,” says Stacie Stephenson, D.C., author of Vibrant: A Groundbreaking Program to Get Energized, Own Your Health, and Glow. Also, “calm, deep breathing reduces stress hormones like cortisol and epinephrine, which can amplify pain signals, and activates those ‘happy brain and body’ hormones such as serotonin and dopamine, which have been shown to have a pain-reducing effect,” Stephenson says. Need a little guidance? Try an app such a Headspace, which includes guided meditations and other mindful techniques.
Practice mind over matter to decrease pain. “There is a huge body of research demonstrating that meditation and other mindfulness practices reduce inflammation,” says Stacie Stephenson, D.C., author of Vibrant: A Groundbreaking Program to Get Energized, Own Your Health, and Glow. Also, “calm, deep breathing reduces stress hormones like cortisol and epinephrine, which can amplify pain signals, and activates those ‘happy brain and body’ hormones such as serotonin and dopamine, which have been shown to have a pain-reducing effect,” Stephenson says. Need a little guidance? Try an app such a Headspace, which includes guided meditations and other mindful techniques.
Exercise
 We know; when you’re stiff, moving your body may be the last thing you feel like doing, but often the stiffness, fatigue, and muscle weakness stem from not moving enough, says Dr. Barkhodari. It doesn’t have to be intense or complicated. Start with our stretches above, then simply walk, he says. “A walking aid or shoe inserts will help to avoid undue stress on your feet, ankles, or knees that have been affected by arthritis,” he says. See a podiatrist to find out if you can benefit from custom-made inserts or ask for a recommendation for store-bought ones to help address your specific issues. Cycling, yoga, and swimming are other low-impact exercises that won’t put stress on your achy joints.
We know; when you’re stiff, moving your body may be the last thing you feel like doing, but often the stiffness, fatigue, and muscle weakness stem from not moving enough, says Dr. Barkhodari. It doesn’t have to be intense or complicated. Start with our stretches above, then simply walk, he says. “A walking aid or shoe inserts will help to avoid undue stress on your feet, ankles, or knees that have been affected by arthritis,” he says. See a podiatrist to find out if you can benefit from custom-made inserts or ask for a recommendation for store-bought ones to help address your specific issues. Cycling, yoga, and swimming are other low-impact exercises that won’t put stress on your achy joints.
Diet
 It’s not a quick fix for pain, but what you eat can help lower your inflammation levels, which can then help relieve symptoms. PsA experts suggest a Mediterranean-style diet, which is rich in antioxidants and omega-3 fatty acids (fruits, vegetables, fatty fish such as salmon and cod, nuts, and extra-virgin olive oil). These foods work to reduce inflammation in the body, while a diet heavy with red meat and processed foods has been shown to do the opposite.
It’s not a quick fix for pain, but what you eat can help lower your inflammation levels, which can then help relieve symptoms. PsA experts suggest a Mediterranean-style diet, which is rich in antioxidants and omega-3 fatty acids (fruits, vegetables, fatty fish such as salmon and cod, nuts, and extra-virgin olive oil). These foods work to reduce inflammation in the body, while a diet heavy with red meat and processed foods has been shown to do the opposite.
For centuries, meditation has been used to quiet the mind and soothe the soul.
A Quick Mini-Meditation to Calm the Body and Mind
This easy five-step mindfulness practice hits the stress relief spot when you don’t have a lot of time to spare.
